Common causes
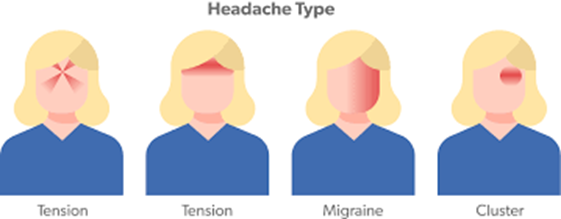
Think about the symptoms that Sadie has and what type of headache she is likely to have.
3 points when assessing headache;
- Is this a red flag.
- Does this need urgent investigations?
- Can this be dealt with in Primary Care?
History taking – things to think about.
Q Why is Sadie consulting now?
A. Her father’s best friend has just died from a brain tumour.
Q What concerns does Sadie have about this headache?
A. Although an underlying brain tumour is rare, it is invariably a concern for both patient and practitioner.
Q How many types of headache does Sadie have?
A. Often people will present with a number of different types. If one type is migraine, the others are likely to be part of a migraine spectrum.
Q Is the headache progressive?
A. A worsening headache can mean that there is something to be concerned about.
Q Ask Sadie about how this affects her day to day life?
A. She is missing social events and having to have time off work.
Q Is there a family history?
A. Migraines can run in families.
Q Ask Sadie what she does when she has the headache, this can give a clue as to the type. People with migraine will want to lie in a dark quiet room, people with cluster headache will pace the room and be agitated, tension-type headache will have little influence on activity.
A. Sadie likes to lie in a dark room and wear sunglasses or a peaked cap if in the daylight.
What has she taken to help the pain and when? Exclude medication overuse headache. This will occur if over a three-month period or longer the patient is taking analgesics on 15 days a month or triptans on more than 10 days.
- Are there precipitating or relieving factors? Relief by lying flat could indicate a low-pressure headache due to reduced CSF pressure.
- A history of other medical conditions is important. There are many comorbidities associated with migraine, in particular anxiety, depression, sleep disorder, and other painful syndromes such as irritable bowel syndrome and fibromyalgia.
